Several weeks ago, an email from a colleague arrived in my inbox with an interesting attachment – an article from the International Journal of Surgery that reviewed the validity of studies using virtual reality to improve training for surgery of the ear, nose and throat (ENT). The article piqued my interest, because my colleagues at the Ohio Supercomputer Center, Don Stredney and his research team in the Interface Lab, have been working with medical professionals for nearly two decades in the development of such a surgical simulator. So, I read a little further.

The authors, led by Dr. Asit Arora of St. Mary’s Hospital in London, and his co-investigators screened 409 abstracts, narrowing their focus to 36 articles on ENT surgery simulations, 21 of which featured surgical simulations of the skull’s temporal bone. On the third page of the study, I noticed why I had received the email – the study included our “OSU temporal bone simulator.” I read on.
The authors ‘summary evaluation of the studies and their ability to predict the validity of their training approaches said this about the OSU study: “The cadaver temporal bone is an excellent model for evaluating skills and represents the gold standard in this regard. The OSU study is the largest randomised validation paper of VR simulation in the literature. It demonstrated equivalence to the gold standard.”
That quote sounded like high praise, so I decided to look into why the compliment had been offered.
First, a bit of background: In 1994, Dr. Gregory Wiet, M.D., of Nationwide Children’s Hospital, received a grant from the National Institutes of Health to lead a multi-institutional study to develop and evaluate a virtual environment for training resident physicians in the techniques of temporal bone surgery. The temporal bone is found along the base and sides of the skull and directly underneath the temple. Sometimes, certain disorders of the ear require surgeons to remove a small section of one of the four pieces of the temporal bone – the mastoid.
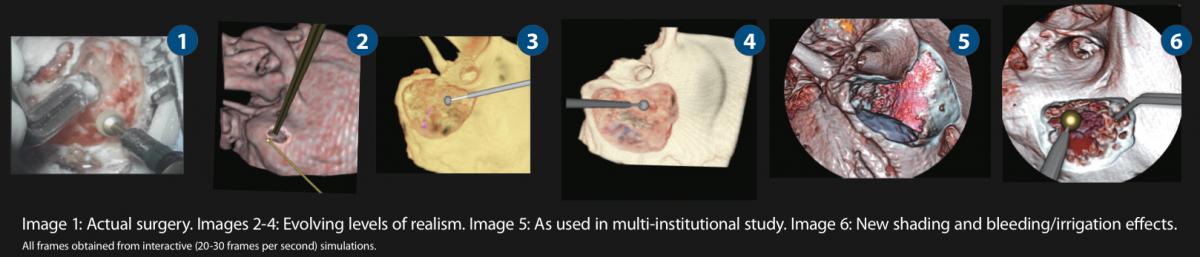
Wiet teamed up with Stredney, who had the computational horsepower and expertise of OSC to help develop models of the simulation environment on a supercomputer. Each iteration of the simulation would then be reduced and configured to run efficiently on desktop computers, laptops and, most recently, tablets. The primary research goals include developing a system that reduces the cost of training, helps surgeons maintain their skills, allows doctors to practice the dangerous techniques in a no-ramification environment, and permits the prudent use of limited resources (cadavers), especially in the initial phases of surgeon training.

In 2008, the research team received the prestigious “Dr. Frank H. Netter Award for Special Contributions to Medical Education” from the Vesalius Trust for Visual Communication in Health Sciences for a pilot phase of the investigation.
Stredney’s particular area of research involves applying high performance computing and advanced interface technologies to develop more intuitive methods for people to use in their interactions with large and complex data sets. Stredney’s research team includes Thomas Kerwin, Ph.D., a research scientist interested in the computer visualization of applications such as simulated surgeries and educational games, and Brad Hittle, a research associate who specializes in software engineering of virtual systems and virtual-reality based simulations for medical applications.
I asked Don why he thought their Temporal Bone simulation had garnered accolades, such as those in the Arora paper. He noted that the paper focused on the validity of such studies and pointed out that the OSU study was designed from the beginning to be a multi-institutional investigation. The study currently includes evaluations from 11 sites “and counting,” as additional institutions continue to ask to become involved, and input from more than 180 subjects.
“This allowed us to get a higher number of subjects to achieve statistical validity, rather than just generalized feedback from a few subjects,” he said.
The researcher team is trying to establish validity in a couple of different ways, he explained. In addition to wanting to know if the virtual environment provides an effective teaching tool, they also are evaluating an automated assessment tool that compares student results to dozens of evaluations provided by veteran ENT surgeons.
I then asked Don what he thought of the praise the Arora article paid them. He simply said, “It’s nice. It’s the result of a lot of work.”
The work on the Temporal Bone surgical simulation isn’t yet complete. The researchers are currently in the fourth of five years of renewable grant funding, and they continue to refine the grading features, enhance the realism of the tools and enlarge the library of available specimens. In fact, the team has recently released Version 2.0 of the software and datasets, and I expect I’ll soon be reading more about the project.



